Introduction
“The best time to plant a tree is twenty years ago. The second best time is now.”
Chinese Proverb
If you are reading this book, it is more than likely that you or someone you know have at one time or another, experienced the sensation of being short of breath due to respiratory disease, cardiovascular disease or both. Shortness of breath (SOB), also known as dyspnea (pronounced disp-nee-uh) or air hunger (pronounced air hun-ger), can be all encompassing and has the potential to undermine every aspect of your life, from the magnificent to the mundane.
There are few sensations in life that are as absolutely terrifying as not being able to catch your breath. In fact, most of us will do absolutely everything in our power to avoid that sensation at all costs, even at the expense of things we love, such as going to the theater, visiting with friends and family; even everyday activities such as taking a shower or grocery shopping; even having sex. Shortness of breath can deliver a tremendous blow to our self-esteem as well as our overall quality of life, but I don’t have to tell you these things. You already know them because you or someone you know has experienced them firsthand, and there are few greater teachers in life than firsthand experience.
My mission in writing this book is to teach you that for the overwhelming majority of people, being diagnosed with a respiratory disease is not a death sentence and your situation does not have to be hopeless, nor should it be. In fact, there are many things you can do to minimize your shortness of breath as well as to maximize your overall health and quality of life.
My mission in writing this book is not to sell you a bill of goods promising a quick fix or cure for your disease or an overnight solution to your shortness of breath. You didn’t get here overnight. You’re not getting out overnight either. I’m also not suggesting that managing your disease will be easy. It will not. I repeat. Managing your pulmonary disease will not be easy. But…if you follow the suggestions in this book, even some of the suggestions, some of the time, I promise you that you will begin to experience small (and in many cases, not so small) but noticeable improvements in your daily life, whether it be less shortness of breath, the ability to do more of the things you love, increased energy levels, or an improvement in your overall sense of well-being.
This is not something I think. This is something I know from firsthand experience because I have seen it work time and time again over the course of my 25-year career as a cardiopulmonary physical therapist, taking care of patients just like you or someone you love.
Many of the suggestions in this book will work for many, if not most people reading it. However, it is important to understand that when it comes to patient care and people in general, all of us are different and therefore, need to be treated as individuals. As such, there will always be exceptions to the rule that will require some adjustments or “tinkering” with the methodology.
SOB or dyspnea on exertion (DOE) is by far, the single most common presenting symptom of respiratory disease and almost always the symptom that causes people to seek medical attention and my assistance. However, it is extremely important to note that shortness of breath can also be the consequence of many conditions besides respiratory disease; ranging in severity from the very serious, like cardiovascular disease, anemia, or renal disease; to the more benign, but still important-to-address conditions like gastro-esophageal reflux disease (GERD) or deconditioning due to inactivity (i.e. being out of shape); or it could be related to something else entirely.
My point in telling you this is that I don’t want you to make any assumptions or self-diagnoses as to the cause of your shortness of breath, without being sure that there aren’t other contributing factors that can potentially be harmful to you if left untreated. With that in mind, it is absolutely essential that your physician perform a comprehensive workup of your symptoms before beginning any meaningful course of treatment or undertaking any significant lifestyle change such as cardiopulmonary physical therapy or pulmonary rehabilitation.
SOB can range in severity from barely noticeable to all encompassing. At times, you may not even be aware of your symptoms while at others, they may stop you dead (or at least, completely breathless) in your tracks. Depending upon where you are, what you happen to be doing, even who you happen to be with at the time, you may attempt to minimize or make light of your symptoms. You may even tell yourself (and others) little white lies such as: “I’m getting old” or “I’m out of shape” or “it’s not a big deal.” But, you know darn well it is. When I hear people use phrases like “it’s not a big deal,” I am reminded of that famous river in northeast Africa called: “the Nile.” Denial, get it?
Typically, most people first begin to experience shortness of breath at high levels of exertion, during activities such as stair climbing or walking uphill. In New York City, the three things patients complain about most are climbing subway stairs, walking up the city’s many hills and inclines and running or walking quickly for the bus; or what we not-so-affectionately like to call “the NYC Pulmonary Triathlon.”
Human nature dictates that when we start to experience a certain symptom; any symptom, whether it be shortness of breath, chest pain, back, hip or knee pain; or any other physical (or emotional) distress, we will typically find ways to alleviate or minimize our discomfort; either by modifying the activity that causes us to be symptomatic (e.g. walking more slowly or taking more frequent rest breaks), or by avoiding the activity altogether (e.g. taking a different route or driving, instead of walking uphill or climbing the stairs).
Therein lies at least part of the problem. The fact is, once you start to avoid the activities that cause you discomfort (whether they be stair climbing, walking uphill or running for the bus), all of the muscles that you use to perform these activities (including, most importantly, the heart; as well as the respiratory and skeletal muscles), become weaker and more deconditioned. And when muscles become deconditioned, they don’t perform as well or use oxygen as efficiently. As a result, you begin to experience shortness of breath at lower levels of activity, and eventually, start to avoid those lower level activities as well and so on and so on. This is what is known as the “Dyspnea Cycle.”
In addition to the muscles themselves, all of the body systems that are involved in performing these activities also become less efficient and when these systems don’t operate as well, guess what. You become even shorter of breath at even lower levels of activity and in turn, start to avoid those activities as well, beginning the cycle all over again. Sound familiar?
At the Pulmonary Wellness & Rehabilitation Center (whether in person or via the Ultimate Pulmonary Wellness Webinar Series, Ultimate Pulmonary Wellness Facebook Group, or this book), our goal is to help you break this cycle in three ways. First, we teach you more effective breathing techniques designed to increase your awareness of and give you greater control over your shortness of breath. Second, we will teach you how to exercise, both aerobically (e.g. treadmill, exercise bike, upper body ergometer) and anaerobically (e.g. strength training), so that your body becomes stronger and more efficient at using oxygen and you become less short of breath.
Last, but definitely not least, we will educate you about the various lifestyle factors that play a role in how well or how poorly you breathe, so that you can begin to reverse your shortness of breath as well as any other limitations or modifications you’ve had to make and that have wreaked so much havoc in your life.
With this principle in mind, my purpose in writing this book is not to give you a complex list of instructions or fancy protocols that are difficult to understand and virtually impossible to follow. Instead, my goal is to present you with a wealth of information that my patients and I have found to be both successful and practical over the past 25 years.
Again, each person is different and every situation is unique. Therefore, not all things will work for all people. However, my hope is that this information will help guide you and your healthcare team in determining which tools and techniques will work best for you and which ones won’t be as helpful, or not helpful at all.
As I mentioned earlier, there are few greater teachers than firsthand experience. I am proud to say that the overwhelming majority of what I have learned about pulmonary disease (and its most effective management) has come from my patients. I have been extremely fortunate to be exposed to great instructors and brilliant mentors throughout both my formal education and my professional career but by far, it has been my patients that have been my most instrumental teachers.
I earned my Bachelor of Science in physical therapy in 1992 from the State University of New York Upstate Medical University in Syracuse, New York, with the help of professors like Susan Miller and program director, Chuck Meacci, who truly forced me to reach my full potential; pushing me way past my own limits, albeit, in an extremely compassionate and nurturing way, mind you; much like what we do with our patients. In fact, I am positive there were many times that they believed in me more than I believed in myself, also much like with our patients.
I earned my Doctor of Physical Therapy in 2006 from Dominican College in Blauvelt, NY. I am also board-certified by the American Board of Physical Therapy Specialties in Cardiovascular and Pulmonary Physical Therapy as well as a New York State Emergency Medical Technician (EMT-B).
I was fortunate to have “grown up” professionally at the New York University (now Langone) Medical Center’s Rusk Institute of Rehabilitation Medicine in New York City. I put the words “grown up” in quotes because there are many that might argue the validity of that statement. Anyhoo, my experience at NYU allowed me to develop my clinical skills and figure out not only what I wanted to be doing with myself, but also what I didn’t want to do. I had incredible mentors including doctors, Horacio Pineda, MD, a beloved physiatrist and pioneer of Rusk’s cardiopulmonary rehabilitation program and Mariano Rey, MD, who was not only a brilliant cardiologist but also a mad tactical visionary, always seeing the big picture quickly and knowing how to get things done within a complex medical and political environment.
In 1995, when I was still only 24 years old, these two giants of medicine took a chance by giving me the opportunity to become the chief physical therapist of the Center’s cardiac and pulmonary rehabilitation programs; changing my life forever; despite the fact that the rest of the medical center let out a collective gasp of “Noah?” That was long before texting but if it weren’t, I am sure there would have been a flurry of 3-letter responses like OMG, SMH, WTF…you get the idea but it was Drs. Pineda and Rey who gave me my shot and for that, I will always be grateful.
I‘ve also had the great fortune to be surrounded by amazing colleagues whom I both respect and trust implicitly. Marion Mackles is without question one of the greatest cardiopulmonary and chest physical therapists, and friends that I have ever known. Marion and I met in 1994 and have been working together for more than two decades.
In 1998, she was just crazy enough to join me in opening the Pulmonary Wellness & Rehabilitation Center. At that time, we spent a lot of nervous hours staring at the walls as we waited for our first patients. Most people predicted we’d remain in business for about 3-6 months but I’m proud to say that we’re still going strong nearly 20 years later.
I was also incredibly blessed to have met one of the greatest personal influences of my life, Lawrence Joseph Virgilio, in 1994. Larry and I crossed paths while we were moonlighting on the weekends at Beth Israel Medical Center in NYC. A short time later, he signed on as the weekend physical therapist at NYU’s cardiac rehabilitation program.
Larry was a Fireman with Manhattan’s elite Rescue Squad 18 in the West Village and also a Senior Physical Therapist at the Pulmonary Wellness & Rehabilitation Center. To this day, I have never encountered someone who routinely developed as natural a rapport with patients, and people, in general, as Larry. I mean, this guy would meet a patient once and for weeks after (months, even), that patient would still be asking how he was doing or to send him their regards. After Marion and I left NYU to open the Pulmonary Wellness Center, I was both thrilled and honored to hear Larry’s voice on the phone asking if he could join us.
The kind of things I learned from Larry cannot be taught in books; things like how to stay (or at least appear) calm in an emergency, how to reassure patients even in the most serious circumstances and also, the importance of not getting caught up in the small stuff that life can throw at you. Larry was a true gentleman and a gentle man but believe me. He could also be as tough as nails when he needed to be.
I still have a newspaper clipping in my desk with a picture of Larry leaning over the side of a building hanging on to a construction worker with one arm after the guy’s scaffold collapsed. Larry worked at the Pulmonary Wellness & Rehabilitation Center until September 11, 2001 at 10:28 AM, when he died in the North Tower of the World Trade Center during the single greatest rescue effort in the history of the FDNY.
Another person I am thankful to have worked with is one of my former students, Greg Sweeney, also an outstanding cardiopulmonary physical therapist, who at the time of this writing is the program manager of NYU’s cardiac and pulmonary rehabilitation program. Over the years, I have watched Greg grow into one of the finest cardiopulmonary therapists and educators in the field. In 2013, Greg and I developed and co-taught a Continuing Medical Education (CME) course called “Cardiovascular of the Rehabilitation Patient,” a primer on the implications of cardiovascular system and heart disease on rehabilitation.
Of course, I also have to credit my parents, Sherry and Mel Greenspan, and my sisters, Erika and Farrah, who have always supported me in whatever endeavor I chose to undertake, as well as my brother David, who understood instinctively that there will never be a shortage of people in the world that need our help.
I also have to pay the greatest homage to my Grandma Peppie, who was by far, the kindest; most generous and most supportive person I have known…ever. I can honestly say that without her, I wouldn’t be the person I am today. In her eyes, I could do no wrong. If someone asked her who did something, she would be like: “I don’t know who did it but I know who didn’t do it, my Noah.”
Since opening the Pulmonary Wellness & Rehabilitation Center in 1998, we have conducted over 85,000 exercise sessions and at this point, I can confidently say that we pretty much have it down to a science. For that, I am grateful for the loyalty and dedication of my team including Marion, Akua Adu-Labi, Aastha Joshi, Wai Chin, Patricia Rocco, Melina Francis, and Caroline Kelley, as well as many others that have spent some time with us over the years; as well as the many physicians, who have honored us with the privilege of caring for their patients.
One such physician is Dr. Norma Braun, MD, who has honored me with her foreword to this book. I have been hearing legendary tales of Dr. Braun’s unconventional methods for decades; including her spending hours on end sitting by her patients’ bedside while they are weaned from a ventilator or going back to their birth in reviewing their medical histories. When I say unconventional, I mean this with the highest possible respect and admiration although it doesn’t really do justice to this medical giant whose compassionate patient care is equally matched by her tenacity in getting to the bottom of each patient’s problem; and then stopping at nothing to address each problem one by one. Gregory House, MD has nothing on Dr. Braun.
I want to thank Mark Mangus, Sr., BSRC, RRT, RPFT, FAARC, who I refer to as the respiratory therapist laureate. Few clinicians have the absolute wealth of knowledge and experience that Mark does. In addition to spending time with us at the Center, Mark has been an invaluable contributor to this book and co-author of the chapter on medications.
I also want to thank Nicole Speletic, Ph.D., a gifted writer and deep thinker, who added a great deal of texture to the fabric of this book, Rena Miller, my Co-Admin of the Ultimate Pulmonary Wellness Facebook Group, who is great at helping to “keep the main thing the main thing,” and Sylvia Johnson, who was a late-game editing blessing.
Finally, last but never, ever least, I must once again acknowledge my many patients, who are by far the driving force behind who I am as a clinician and who I strive to be as a human being. It is through these symbiotic relationships, with the very people who come to me for help; allowing me to participate in their lives and getting to know them through their disease; that I am constantly learning about myself and continuing to grow, both professionally and personally.
In sharing our collective experience with you, I hope to give you a direct link to the greatest source of information about your disease, in an effort to help you avoid some of the same pitfalls that others before you have had to deal with. One thing that I can tell you for certain is that even more gratifying than trial and error; is trial and success, especially when it comes to my patients.
The good news is that the overwhelming majority of the information being passed on to you has come directly from the source: other patients. They are the true experts in the field, who have experienced many of the same struggles as you and found ways to overcome them, even when it seemed like all odds were against them and you can too. It is my hope that by putting our collective knowledge and experience together in one comprehensive, yet easy to understand “bible” for pulmonary patients, you will have at your disposal, a wealth of options to choose from, and that you too, will be able to experience your own little slice of “Ultimate Pulmonary Wellness.”
Nothing in the world gives me greater satisfaction than helping people breathe better, to feel well instead of sick, and to truly live their lives instead of watching it pass them by from the sidelines. A big part of that involves clearing up confusion about their disease and dispelling myths and misinformation (of which, there is a lot), an unfortunate but not uncommon byproduct of today’s fast-paced healthcare environment.
In some ways, the Internet can be one of the best sources of medical information, but in others, it can also be one of the most detrimental, not to mention, terrifying. For one thing, information on the Internet is not always completely accurate or current. Often, it’s not even remotely accurate, and sometimes, people discover far more than they ever wanted to know, often completely out of context and without a proper filter or guide to help them separate fact from fiction.
That’s what I’m here for. I wrote this book to help remedy that precise situation and to help clear up any confusion you may have regarding your disease (or at least point you in the right direction). Ultimate Pulmonary Wellness is meant to be an infinitely and intimately useful guidebook covering the medical, behavioral, and lifestyle issues of not just living; but living well and thriving, despite your pulmonary condition.
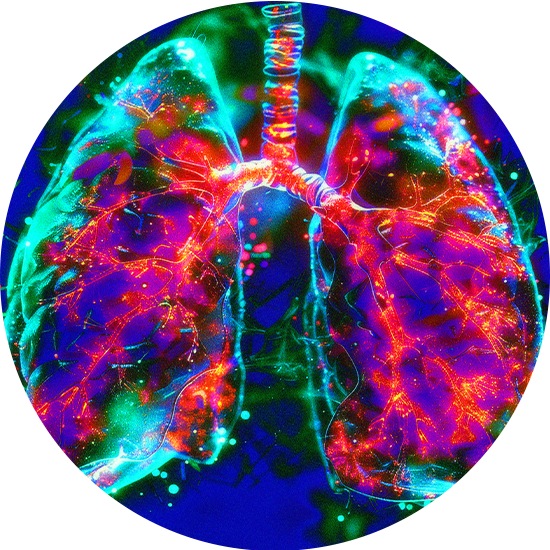
On this journey, I will cover some of the basics, taking you on a quick tour of the functional anatomy and physiology of the respiratory system as well as some key components of the cardiovascular system. I will also guide you through the diagnostic process, explaining some of the many tests and procedures you may undergo, as well as some of the more commonly used medical practices and interventions.
We will also go through what I believe are the five key components of Ultimate Pulmonary Wellness: Medical, including finding the right doctor, taking the right medications, and taking them properly; Exercise, Nutrition, Stress and Anxiety Management/Meditation; and Prevention of Infection.
As for smoking, you know what you have to do. As Nike says, “Just Do It” (or in the case of smoking, just don’t do it). That includes cigars, pipes, hookah, and “e-cigarettes.”
In this book, you will find useful, proven tips, as well as images, charts and worksheets that you can use to record notes and track your progress. I’ve also included a glossary of key terms because there’s nothing more frustrating than when medical professionals use fancy jargon or complicated medical terms without a corresponding “Gibberish to English” dictionary.
I’m so thankful that you have decided to read this book and to take the first steps in making your life better. This means more than simply not being short of breath, or learning how to live with your disease and its associated symptoms. Instead, it means setting out on a path to truly becoming your best self and to achieving your own state of Ultimate Pulmonary Wellness.
I wish you all the best in life and hope that if you’re in New York City, you’ll stop by the Center. We play great music, sing karaoke, and have amazing art on the walls. We have beautiful fish and the greatest dog named Monkey. We have a lot of laughs and do everything we can to spoil our patients rotten. We also happen to get great results!